Dr. Neil Floch can provide you with a permanent solution to these problems. Dr. Floch is a highly acclaimed laparoscopic pioneer in the procedures, having performed acid reflux surgeries for twelve years and offer Laparoscopic Nissen Fundoplication, Laparoscopic Toupet Fundoplication, Heller Myotomy, and Paraesophageal Hernia Repair surgery. They will offer the safest professional surgical care to help you through the process of reclaiming your life. You will be able to return to a healthy full life eating the foods you love, and doing all of the activities that brought you so much enjoyment before you started to suffer with GERD.
WHEN IS SURGERY CONSIDERED?
Surgery is considered when symptoms do not improve with medications:
- If they repeatedly return after the medication is stopped
- As an alternative to lifelong medication
- If you are unwilling or unable to take medication for prolonged periods
- If there is severe damage to the esophagus due to reflux. A large hiatus hernia, esophageal ulcer, narrowing or change in the lining of the esophagus, such as Barrett’s esophagus may be further indications for surgical therapy.
HOW DOES ANTIREFLUX SURGERY WORK?
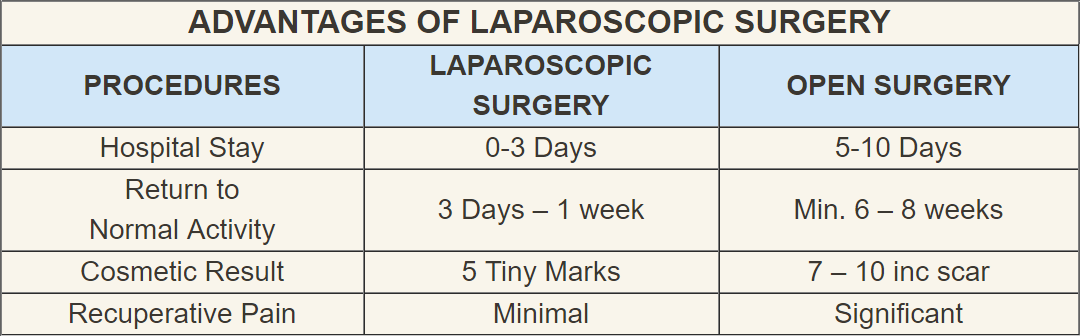
For sixty years surgeons have performed an operation known as a fundoplication to prevent reflux. Before 1991 it was necessary to make a long incision between the breastbone and the “belly button.” This resulted in significant discomfort and a hospital stay of about five to ten days, with an average time for return to normal daily activities of about six to eight weeks.
Since 1991, surgeons have used a laparoscope to do the fundoplication. This is a long, thin telescope the size of a finger, which is placed into the abdomen. Five small incisions, each about a centimeter wide, are used to gain access to the abdomen. Dissecting instruments, thread and other materials can be inserted and removed through these small holes, allowing the surgeon to perform the operation. If there is a hiatus hernia, which is a slippage of part of the stomach through the diaphragm into the chest, this is repaired by pulling the stomach into the “belly.” Then the hole in the diaphragm is sewn closed so that it only allows the esophagus to pass through. A small portion of the upper stomach is loosened from the surrounding tissues and wrapped around the lower esophagus. As a result the valve between the esophagus and the stomach is tightened. The operation is performed in one to three hours.
Other variations of this procedure may be performed. The most common of which is the partial wrap or Toupet in which the stomach is wrapped around two thirds of the lower esophagus. This procedure is used for people who have weakened muscles of the esophagus.
Patients usually have little pain and discomfort after laparoscopic surgery when compared to open surgery; therefore they recover more quickly. Some patients may go home on the day of surgery, but most leave the hospital in one or two days. Return to social and work activities may occur in one to three weeks, which is much sooner than with the open surgical technique.
WHAT ARE THE COMPLICATIONS OF SURGERY?
Surgical complications are rare but do occur in 2 to 4 % of patients who undergo laparoscopic surgery. With any surgery performed under general anesthesia, there is a less than one in a thousand chance of severe complications from the anesthesia medications. There is a less than 1 in 500 possibility of severe bleeding that may require transfusion. All surgeries carry the risk of wound infection, postoperative pneumonia or blood clots forming in the deep veins in the legs. These risks are reduced by the use of antibiotics, anticoagulant medication and the laparoscopic technique, which allows the patient to be active soon after surgery.
There are complications specific to the surgery. Damage to organs such as the stomach, esophagus, spleen or liver may occur. This may or may not be identified by the surgical team during surgery and could result in serious infection, but these problems can usually be repaired at the time of laparoscopic surgery. Tracking of air into the chest cavity or the space around the lungs may occur. In our experience of over 500 cases, complications were rarely encountered and were appropriately handled.
Occasionally it is not possible to complete the operation with the laparoscopic technique because of difficulty with visualization or because of a complication. The need to convert to an open operation with an upper abdominal incision is necessary in less than one in two hundred cases. In Dr. Floch’s experience there have been no mortality or conversions.
Other complications may arise after surgery. If the wrap is too tight there may be persistent difficulty in swallowing. This can occur in 20% of patients immediately after surgery but drops to about 5% after one to two months. Four percent of patients will need dilation of the esophagus. The wrap may slip into the chest or become undone resulting in difficulty swallowing or recurring symptoms. If this occurs, reoperation may be required.
WHAT ARE THE SIDE EFFECTS AFTER SURGERY?
Half of the patients have difficulty eating solid food for several weeks after surgery. This is due to swelling at the site of the stomach wrap. As the swelling goes down, solid food will pass more easily. Belching can create some discomfort. Diarrhea and distention of the “belly” may also occur; all these problems improve with time. The gastric wrap may rarely become too tight or too loose. This may result in the need for medication or further surgery.
HOW IS PAIN CONTROLLED?
Pain from the incisions is common during the first 24 to 48 hours after surgery. You may also experience abdominal discomfort and shoulder pain from retention of carbon dioxide gas in the abdominal cavity. Carbon dioxide gas is used to inflate the abdominal cavity during surgery to allow access to the esophagus, stomach and surrounding organs by the surgical team. Pain medications will be prescribed by your physician while in the hospital and prior to discharge to help relieve this discomfort. You will be given a prescription for a liquid painkiller when you leave the hospital. Narcotics may cause constipation. For relief, we recommend using a stool softener such as Milk of Magnesia or call the doctor’s office for assistance. You should not take narcotic pain medications on an empty stomach or drink alcohol.
WHAT DIET MAY I EAT IN THE HOSPITAL?
The evening after surgery you will be given a clear liquid diet. Take small sips and drink slowly. The newly created valve may be swollen and liquids may move slowly through the esophagus. Swallowing large amounts of liquid or “gulping” may cause chest pain or excessive belching. Occasionally cold or carbonated beverages may also cause chest pain; they should be avoided. The morning after surgery, you may be given a pureed diet. These foods are easily chewed and swallowed.
HOW SHOULD I CARE FOR MY WOUNDS?
There are usually 5 small abdominal incisions; each is covered by steri-strips and translucent bandages. These may be removed or left on at discharge from the hospital. Either is acceptable. A small amount of bloody discharge from the incisions is normal and is usually seen through the bandage. You may shower immediately if you have the translucent bandages. Steri-strips will be removed in our office at your first postoperative visit. If they fall off they do not need to be replaced.
WHAT MAY I EAT AT HOME?
When you arrive home you should remain on liquids and pureed food for one week. You may eat cereal with milk, soups, tuna fish, mashed potatoes, banana, milk shakes, and cottage cheese. In the second week you will be advanced to cooked vegetables, toasted bread, cereal with milk, pasta and cooked fish. In the third to fourth week you may be advanced to: dry bread, chunks of meat, hard fruits such as melon and apple and dry foods such as crackers. If you encounter a food that sticks in your esophagus, go back to eating softer foods for a few days. As the swelling in the esophagus subsides solid food is better tolerated. Most patients can eat all foods by 3-4 weeks following surgery.
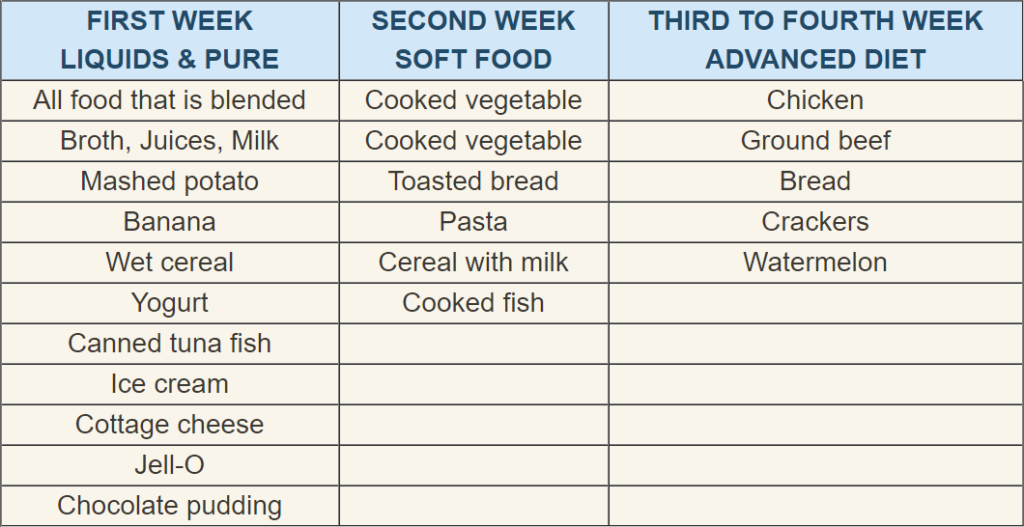
Boost or Ensure may be used in the first two week to supplement your diet and prevent weight loss
**Remember a 10 lb. weight loss is the average during this period
HOW SHOULD I EAT?
The way you eat after surgery is as important as the foods you eat. With all meals, but particularly with foods like bread, steak, and chicken, eat slowly, take small bites, and follow with sips of liquid. Allow each bite to pass through the esophagus to the stomach before swallowing the next. Eating too much food, too fast may cause a delay in the passage of food for several seconds, causing pain and occasionally vomiting. A few bites of food or sips of liquid may fill the stomach, because part of the stomach was used in creating the new valve and the capacity of the stomach is smaller. This is a temporary condition because the stomach tends to dilate to its original size over a few weeks. In this period, plan to eat 5-6 small meals per day, instead of 3 larger meals.
WHEN MAY I RESUME REGULAR ACTIVITY?
All usual physical activity may be resumed as indicated by your ability. Initially, you will be tired after short periods of activity, but in time your energy level will increase. This is normal. Remember that although you do not have a large incision, you have had major surgery, so plan on frequent rest periods. You may expect to return to your normal activity level and resume work in about 1-2 weeks depending upon your type of work. You may drive about one week after hospital discharge. More importantly, you must feel well, be off narcotic pain medications and be able to move your feet to press the pedal. Remember that you are responsible for your safety, as well as that of others on the road. If you feel you would like to participate in sports, please contact your doctor. If you are still in school, you may go back to school about one week after you have been discharged.
WHAT SHOULD I BE CONCERNED ABOUT?
The doctor or nurse should be notified if you experience the following: discomfort that becomes worse or is severe, excessive drainage from the incisions, redness or swelling of the incisions, temperature greater than 101.5 degrees Fahrenheit, nausea, vomiting, diarrhea or constipation which continues for more than 1 to 2 days. You are also encouraged to talk to your surgeon or nurse if you have any questions about your surgery or recovery.